Adult Medical
General Approach to All Patients
Abdominal Pain/GI Bleeding
Acute Adrenal Insufficiency
Airway Emergencies-Adult Dyspnea
Diabetic Emergencies
Drowning
Foreign Body Obstruction
Respiratory Failure
Pharmacologically Assisted Intubation
Confirmation of Airway Placement
Allergic Reactions
Altered Mental Status
Behavioral Emergencies
Hypertensive Emergencies
Hyperthermia
Hypothermia
Pain Management
Sedation/Sedative Agent Use
Seizure
Sepsis
Shock
Stroke - Suspected
Syncope
Tracheostomy Complications
General Approach to All Patients
The following measure will apply to the management of all patients:
Basic Life Support
- Establish patent airway
- Supplemental oxygen if any respiratory signs or symptoms present
- Including ETCO2 level (35-45 normal)
- Record and monitor vital signs
- Record blood glucose level if any weakness, altered mental status or history of diabetes
- Nothing by mouth, unless patient is a known diabetic with hypoglycemia and is able to self-administer oral glucose paste, or a glucose containing beverage
Advanced Life Support
- When condition warrants (specified as “Full ALS Assessment and Treatment” in individual protocols):
- Advanced airway/ventilatory management as needed
- Perform cardiac monitoring
- Evaluate 12-lead ECG especially if chest pain, dyspnea, abdominal pain above the umbilicus or ischemic equivalent symptoms (nausea, dizziness, palpitations) (to be completed within first 5 mins of patient contact)
- If STEMI criteria present on 12 lead ECG, transmit ECG to PCI capable hospital and expedite transport (see Chest Pain protocol)
- Record & monitor continuous 02 saturation and microstream capnography
- IV 0.9% NaCl KVO or IV lock
- If evidence of dehydration (tachycardia, dry mucous membranes, poor skin turgor) administer boluses of 0.9% NaCl at 250 ml (hold at 500 ml total if no hypotension)
- If BP < 90 mm Hg systolic, administer boluses of 0.9% NaCl at 250 ml until systolic BP > 90 mm Hg
- Contraindicated if evidence of congestive heart failure (e.g. rales)
- If hypoglycemic (Blood glucose < 70 mg/dL (<50mg/dL if stroke)):
- Dextrose 10% 100ml IV/IO, (repeat in 10 minutes if BGL remains < 60) max of 250ml
- If no IV available:
- Glucose paste or other oral glucose containing agent (e.g. orange juice) if patient alert enough to self administer oral agent
- If unable to take oral glucose administer Glucagon 1 mg IM/IN
- For patients with severe nausea or vomiting:
- Ondansetron (Zofran), 4 mg slow IV/IM or 4 mg Oral Disintegrating Tablet (ODT) by mouth
- Transport patient to nearest appropriate Emergency Department
- Minimize on scene time when possible
Contact Medical Control for Additional Orders if Needed
Abdominal Pain/GI Bleeding
Basic Life Support
- Nothing by mouth
Advanced Life Support
- If pain above the umbilicus perform cardiac monitoring and 12 lead ECG
- IV 0.9% NaCl KVO or IV lock
- If evidence of dehydration (tachycardia, dry mucous membranes, poor skin turgor) administer boluses of 0.9% NaCl at 250 ml (hold at 500 ml total if no hypotension)
- For patients with severe nausea or vomiting
- Ondansetron (Zofran), 4 mg slow IV/IM or 4 mg Oral Disintegrating Tablet (ODT) by mouth
- Hold in 1st trimester of pregnancy if pregnancy if documented
- Ondansetron (Zofran), 4 mg slow IV/IM or 4 mg Oral Disintegrating Tablet (ODT) by mouth
Kidney Stone Highly Suspected
- Limit treatment to patients meeting the following criteria:
- Age ≤ 65 years
- Not known to be currently pregnant
- Prior history of kidney stone
- Pain consistent with prior kidney stone episodes
- Pain isolated to the flank with or without radiation to the groin
- No history of fever (> 100.4 F)
- Systolic blood pressure ≥ 120
- No abdominal mass or significant tenderness
- No trauma suspected
- Positive distal pedal pulses
- For patients with severe pain meeting the Kidney Stone criteria above:
- Fentanyl (Sublimaze) 1 mcg/kg (maximum 100 mcg) slow IV; repeat once after 5 minutes as needed (maximum 200 mcg total dose) OR 100 mcg intranasal via MAD (divide dose equally between each nare)
Contact Medical Control for Additional Orders if Needed
Acute Adrenal Insufficiency
Acute adrenal insufficiency or Addison’s disease is an endocrine disorder that occurs when the adrenal glands do not produce sufficient amount of cortisol and other glucocorticoid hormones needed to respond to stress and inflammatory reactions and needed to re-establish homeostasis after a stress response.
Early signs and symptoms of patients in acute adrenal crisis include pallor, dizziness, headache, weakness/lethargy, abdominal pain, nausea/vomiting and hypoglycemia. If left untreated, symptoms may progress to hypotension, shock, seizure and eventual heart failure.
Basic Life Support
- Supplemental 100% Oxygen to maintain O2 saturation > 95%
- Including ETCO2 level (35-45 normal)
- Record and monitor glucose levels
- Record and monitor vital signs including temperature
Advanced Life Support
- Record and evaluate 12 lead EKG
- IV 0.9% NaCl or IV lock
- If indicated (i.e. tachycardia, hypotension), 20 ml/kg NaCl to maintain systolic BP ≥ 90 mmHg
- For patient’s confirmed to have acute adrenal insufficiency by either the presence of a medical alert bracelet, designation of medical records or other patient, family or medical confirmations
- Contact Medical Control to advise of patient’s condition and request to administer the following:
- Patient’s Solu-Cortef if present
- If Solu-cortef not available, administer Solu-Medrol 125mg slow IV push
- Contact Medical Control to advise of patient’s condition and request to administer the following:
Contact Medical Control for Additional Orders if Needed
Airway Emergencies - Adult Dyspnea
Basic Life Support
- Supplemental 100% oxygen
- Including ETCO2 level (35-45 normal)
Advanced Life Support
- Full ALS Assessment and Treatment
- Including ETCO2 level (35-45 normal)
- Observe for signs of impending respiratory failure; refer to Respiratory Failure section if needed
- Hypoxia (O2 sat < 90) not improved with 100% Oxygen
- Poor ventilatory effort (increasing ETCO2 not improved with treatment)
- Altered mental status/ decreased level of consciousness
- Inability to maintain patent airway.
- Begin CPAP if initial symptoms are severe (refer to CPAP procedures)
- Based on presentation, use manufacturer settings for Asthma/COPD or CHF
- Brief interruptions to administer medications are acceptable
Acute Bronchospasm (wheezing or history of asthma or COPD)
- Albuterol (Proventil) 2.5 mg/3 ml and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer
- Repeat Albuterol (Proventil)/Ipratropium Bromide (Atrovent) X 2 if wheezing persists
- Methylprednisolone (Solumedrol) 125 mg IV if wheezing persists after 1st nebulizer
- If not improving, Magnesium Sulfate 2 grams IV in 100 ml NS over 10-15 minutes
- Contraindicated if hypotensive or history of renal failure
- Do not use if CHF suspected
- If SEVERE respiratory distress and wheezing persists after above:
- Epinephrine 1:1,000 0.3 mg IM (consider consultation with Medical Control if patient >55 years old, known to be on B blockers or known coronary artery disease)
Acute Pulmonary Edema (history of CHF, pedal edema, elevated SBP)
- Nitroglycerin 0.4 mg spray/tablet SL every 5 minutes (max 3 doses)
- Contraindicated if systolic BP < 90 mm Hg
- Contraindicated if use of a Phosphodiesterase-5 (PDE5) inhibitor use within last 24 hours (Viagra or Levitra); 48 hours for Cialis
- Contraindicated if EKG changes consistent with ischemia in the inferior leads or signs of infarct
- For bronchospasm (wheezing) associated with Acute Pulmonary Edema
- Albuterol (Proventil) 2.5 mg/3 ml and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer
- Repeat Albuterol (Proventil)/Ipratropium Bromide (Atrovent) X 2 if wheezing persists
- Albuterol (Proventil) 2.5 mg/3 ml and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer
- For hypotension (systolic BP < 90 mmHg)
- Norepinephrine infusion at 0.5-16 mcg/minute IV/IO, titrated to maintain SBP > 90 mm Hg (see pg. 10-27 for infusion preparation chart) if available OR
- Administer push dose Epinephrine titrated to SBP>90 mm Hg or max dose (10ml) reached OR
- Epinephrine infusion at 2-10 mcg/min IV/IO, titrated to maintain SBP > 90 mm Hg (see pg. 10-14 for infusion preparation chart)
Diabetic Emergencies
Hypoglycemia
- If hypoglycemic (Blood glucose < 70 mg/dL (<50mg/dL if stroke)):
- Dextrose 10% 100ml IV/IO, (repeat in 10 minutes if BGL remains < 60 mg/dl) max of 250ml
- If no IV available:
- Glucose paste or other oral glucose containing agent (e.g. orange juice) if patient alert enough to self-administer oral agent
- If unable to take oral glucose administer Glucagon 1 mg IM/IN
- When available, give 1 amp (25 g) of D50 for hypoglycemia in cardiac arrest
- If hypoglycemia persists:
- Repeat blood glucose check with a different glucometer (if available)
- ALS Assessment for underlying conditions (i.e. infection, sepsis, MI, stroke)
Hyperglycemia
Causes: Illness, infection, ischemia (stroke or MI), insulin (lack of), drug/alcohol abuse
Signs/Symptoms: (includes but not limited to) weakness, dizziness, seizure, nausea, vomiting, tachypnea, polyuria (frequent urination, & polydipsia (thirst)
* Patients with prolonged and/or severe hyperglycemia are at risk for significant volume losses leading to dehydration and electrolyte abnormalities
If blood glucose level is 300-500mg/dL:
- ALS Assessment for underlying conditions
- Obtain EKG
- Assess ETCO2. If ETCO2 <29 suspect DKA. If ETCO2 is >30 not likely DKA.
If blood glucose level is >500 or “High”:
- ALS Assessment for underlying conditions
- Obtain EKG
- Assess ETCO2. If ETCO2 is <29 suspect DKA. If ETCO2 is >30 not likely DKA.
- Administer IV fluid bolus in the absence of CHF
Diabetic Ketoacidosis >300 mg/dL and end tidal <29
- Initiate IV access
- Administer NS Bolus up to 1000L in the absence of CHF. Reassess after 250ml increments for evidence of pulmonary edema. Discontinue infusion if pulmonary edema develops.
- Transport ALS to the closest appropriate hospital (not a freestanding).
Drowning
- Spinal immobilization if indicated
- Consider CPAP for patients with significant dyspnea or hypoxia
- Protect from heat loss
- Patients may develop delayed onset respiratory symptoms
- Refer to appropriate protocol if cardiac arrest present
Foreign Body Obstruction Suspected
- Perform obstructed airway procedures per BLS standard
- Attempt suction and removal with Magill forceps using direct visualization
- Observe for signs of impending respiratory failure
- If unconscious or unresponsive:
- Give a series of 30 chest compressions then inspect for object in mouth prior to attempting breaths
- If unsuccessful after one series of compressions and ventilations, establish direct view of object with laryngoscope and remove with Magill forceps
- If complete obstruction below the vocal cords and FB not removable, then intubate into right mainstem bronchus to advance FB with ETT, then pull back ETT to normal position to ventilate left lung.
Respiratory Failure
Basic Life Support
- If suspicion of trauma, maintain C-spine immobilization
- Suction all debris, secretions from airway
- Supplemental 100% oxygen, then BVM (with OPA/NPA) ventilation if indicated
- Including ETCO2 level (35-45 normal)
Advanced Life Support
- Monitor end-tidal CO2 (capnography 35-45 normal) and oxygen saturation > 94% continuously
- Follow algorithm if invasive airway intervention is indicated (ETT or supraglottic airway):
- Apnea
- Decreased level of consciousness with respiratory failure (i.e. hypoxia (O2 sat <90) not improved by 100% oxygen, and/or respiratory rate < 8)
- Poor ventilatory effort (with hypoxia not improved by 100% oxygen)
- If patient is able to tolerate (no gag reflex) insertion of OPA then advanced airway should be inserted.

- Effective bag valve mask ventilation is an acceptable endpoint unless patient tolerates insertion of OPA, then advanced airway should inserted
- Attempt cricothyrotomy after all other oxygenation/ventilation methods have failed. A Supraglottic device must be attempted prior to a cricothyrotomy.
Contact Medical Control for Additional Orders if Needed
Pharmacologically Assisted Intubation
Basic Life Support
- Preoxygenation
- Administer 100% oxygen to patients for at least 3 minutes prior to intubation when feasible
- Non-rebreather turned to max flow
- BVM, OPA, and NPA if O2 falls below 93%
- Capnography monitoring (ETCO2 level 35-45 normal)
- Apneic oxygenation- Administer O2 via nasal canula during paramedic’s intubation attempts
- Turn to max flow
Advanced Life Support
- Indications for Pharmacologically Assisted Intubation
- Unable to intubate without drug assistance
- Prolonged transport time (> 15 minutes)
- Full ALS Assessment and Treatment
- Monitor oxygen saturation and ETCO2 waveform continuously
- Prepare intubation equipment
- Resuscitate before intubating to prevent hypotension, hypoxia, and cardiac arrest during or post intubation
- if hypotensive give fluids (if tolerable) and a push-dose pressor for temporary improvement prior to administering sedative
- Push dose epinephrine: Remove 9ml (0.9mg) of 1:10,000 Epinephrine from the pre-filled syringe then draw 9ml of NS into the pre-filled syringe and mix solution. Concentration 10mcg/ml. IV push 1ml every minute to increase blood pressure to 90 mmHg; max 10ml (100mcg) in preparation for intubation.
- if hypoxic, vigorously pre-oxygenate to achieve an O2 saturation of 93% or greater prior to administering sedative
- 2 person BVM technique, OPA, or NPA, 100% O2 supplementation, PEEP valve if available
- If acidotic (i.e. end tidal less than 30) administer fluids and limit apnea time during intubation
- **For all conditions above, consider supraglottic or video laryngoscopy due to high success rates and quick time of intubation
- if hypotensive give fluids (if tolerable) and a push-dose pressor for temporary improvement prior to administering sedative
- Have bougie, video laryngoscopy, supraglottic airway and cricothyrotomy kit ready
- For Adult medical patients (age > 10 years)
- Etomidate 0.3mg/kg IV/IO (Max 30 mg)
- For Adult medical patients (age > 10 years)
- For Adult medical, trauma and asthmatic patients (age > 10 years)
- Ketamine 1 mg/kg IV/IO (Max 100 mg)
- If inadequate response or higher dose indicated Contact Medical Control
- Ketamine 1 mg/kg IV/IO (Max 100 mg)
- Intubate patient with endotracheal tube
- Position patient's head so that the ear is parallel and in line with the sternal notch
- Oxygenate between intubation attempts
- Abort attempt if O2 decreases below 90%
- Max 1 attempts for trauma patients (consider VL as 1st attempt); if unsuccessful proceed to supraglottic airway or BVM
- Max 2 attempts for medical patients; if 1st attempt fails, 2nd must be with Video Laryngoscopy (VL)
- Confirm tube placement
- Continuous ETCO2 waveform monitoring
- Direct visualization
- Condensation in the tube
- Auscultation
- Chest rise and fall
- After successful intubation confirmed, if sedation needed; may administer one of the following meds:
- Versed 2.5mg IV/IO if bp greater than 120
- Etomidate 0.3mg IV/IO (max 30mg)
- Ketamine 0.5mg/kg IV/IO (max 50mg)
- Repeat doses can be considered with medical control
- If unable to intubate, attempt intubation with supraglottic airway
- If you are unable to ventilate and provide adequate oxygenation
- Perform cricothyrotomy (again cricothyrotomy is only for patients > 12 years of age)
- For patients who are ≤ 10 years of age, Contact Medical Control prior to administration of pharmacologic agents for assisting intubation.
Medical Control must be notified any time pharmacologically assisted intubation is performed.
Confirmation of Advanced Airway Placement and Effectiveness of Ventilation
Capnography/ETCO2 Monitoring:
- Digital capnography (waveform) is the system standard for ETCO2 monitoring and continuous ETCO2 monitoring is a MANDATORY component of critical patient management as well as invasive airway management
- Immediately after placing an ETT or supraglottic airway, capnography shall be re-applied to confirm proper placement
- Proper placement is indicated by the presence of a continuous alveolar waveform on Capnography (35-45 normal)
- If an alveolar waveform is not initially present, or disappears after 3-5 breaths (i.e. flat-line), remove the ETT or supraglottic airway and proceed to the next step in the algorithm
- If continuous expired ETCO2 cannot be detected by above method, the invasive airway device must be removed, and the airway managed noninvasively
Additional Measures
- Assess epigastric sounds, breath sounds, and chest rise and fall
- Record tube depth and secure in place using a commercial tube holder
- Utilize head restraint devices (i.e. “head-blocks”) or rigid cervical collar and long spine board immobilization as needed to help secure airway device in place
Contact Medical Control for Additional Orders if Needed
Allergic Reactions
Basic Life Support
- Assist patient in self-administration of previously prescribed epinephrine (Epi-Pen)
Advanced Life Support
Mild Reaction (Itching/Hives)
- Diphenhydramine (Benadryl) 1 mg/kg IV (Maximum 50 mg)
- May be administered IM if no IV access available
Moderate Reaction (Dyspnea, Wheezing, Chest tightness)
- Albuterol (Proventil) 2.5 mg/3 ml via and Ipratropium Bromide 0.02% (Atrovent) 0.5mg/2.5 ml via nebulizer
- Repeat Albuterol (Proventil)/Ipratropium Bromide (Atrovent) X 2 for continued wheezing
- Diphenhydramine (Benadryl) 1 mg/kg IV (Maximum 50 mg)
- May be administered IM if no IV access available
- Methylprednisolone (Solumedrol) 125 mg IV/IM
Severe Reaction
(BP < 90 mm Hg, stridor, severe respiratory distress, or lip-tongue swelling) OR ( skin PLUS respiratory symptoms: hives/itching PLUS dyspnea, wheezing or chest tightness) OR (skin or respiratory symptoms PLUS GI symptoms: hives/itching or dypsnea/wheezing PLUS vomiting or abdominal pain) with likely allergen for that patient
- Epinephrine 1:1,000 0.3 mg IM for rapidly progressive worsening of symptoms (consider consultation with Medical Control if patient >55 years old, known to be on B blockers or known coronary artery disease)
- Repeat Epinephrine if signs of severe reaction or shock persist after initial dose
- If patient has signs of shock and blood pressure is <90mm HG after 2 doses of IM epinephrine and fluids, start an epinephrine drip (see chart)
- Albuterol (Proventil) 2.5 mg/3 ml and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 mlvia nebulizer
- Repeat Albuterol (Proventil)/Ipratropium Bromide (Atrovent) X 2 if wheezing persists
- Diphenhydramine (Benadryl) 1 mg/kg IV (Maximum 50 mg)
- May be administered IM if no IV access available
- Methylprednisolone (Solumedrol) 125 mg IV/IM
Cardiac Arrest or Cardiopulmonary Arrest Imminent
- For impending cardiac arrest, Epinephrine 1:10,000 0.5 mg IV/IO (instead of 1:1,000 IM)
- For cardiac arrest, refer to the appropriate protocol based on presenting rhythm
- In the setting of cardiac arrest, the following items should be performed in the post resuscitative phase, when time allows:
- Albuterol (Proventil) 2.5 mg/3 ml and Ipratropium Bromide 0.02% (Atrovent) 0.5mg/2.5 ml via nebulizer
- Repeat Albuterol (Proventil)/Ipratropium Bromide (Atrovent) X 2 if wheezing persists
- Albuterol (Proventil) 2.5 mg/3 ml and Ipratropium Bromide 0.02% (Atrovent) 0.5mg/2.5 ml via nebulizer
- Diphenhydramine (Benadryl) 1 mg/kg IV/IO (Maximum 50 mg)
- Methylprednisolone (Solumedrol) 125 mg IV/IO
Contact Medical Control for Additional Orders if Needed
Altered Mental Status
Advanced Life Support
- Full ALS Assessment and Treatment (to include stroke exam if possible)
- If hypoglycemic (Blood glucose < 70 mg/dL (<50mg/dL if stroke)):
- Dextrose 10% 100ml IV/IO, (repeat in 10 minutes if BGL remains < 60 mg/dl) max of 250ml
- If no IV available:
- Glucose paste or other oral glucose containing agent (e.g. orange juice) if patient alert enough to self administer oral agent
- If unable to take oral glucose administer Glucagon 1 mg IM/IN
- When available, give 1 amp (25 g) of D50 for hypoglycemia in cardiac arrest
- If hypoglycemia persists:
- Repeat blood glucose check with a different glucometer (if available)
- If Opioid overdose suspected (significantly altered mental status or respiratory depression):
- Naloxone (Narcan) 2 mg IV (start at 0.4 mg for patients over 65 years old)
- Naloxone (Narcan) can be given in 0.4 mg increments, titrated to mental status and respiratory drive (monitor respiratory status with continuous capnography)
- If respiratory depression persists, repeat every 3 minutes to a maximum of 8 mg (10mg max if Narcan administered prior to arrival)
- If IV access has not been established, Naloxone (Narcan) can be given IM or via Mucosal Atomizer Device (MAD)
- Naloxone (Narcan) 2 mg IV (start at 0.4 mg for patients over 65 years old)
- If Stroke suspected see Stroke Protocol
- If Sepsis suspected (advanced age, high risk for infection, febrile), see Sepsis Protocol
- If Head Injury suspected see Trauma/Head Injury Protocol
- If severely agitated and/or violent see Behavioral Emergencies Protocol
- If cardiac arrhythmia present see appropriate Cardiac Arrhythmia Protocol
Note: Patients presenting with altered mental status, who respond to Narcan are not candidates for informed refusal. Due to the relatively short half-life of Narcan, these patients are medically incapacitated, and should be transported, regardless of the presence of an apparently normal mental status.
Contact Medical Control for Additional Orders if Needed
Behavioral Emergencies
Basic Life Support
- Apply physical restraints if needed to ensure patient/crew safety
- Restrain patients in supine or lateral recumbent position only, using no excessive force
- Never allow patients to be restrained in the "hog-tied" or prone position
- Continuous cardiac, O2, and end tidal Co2 monitoring is required when a physical or chemical restraint is utilized
Advanced Life Support
- When chemical or physical restraints are used perform Full ALS Assessment and Treatment and call for safety alert
- For patients with severe agitation compromising patient care or patient/crew safety, or for patients who continue to struggle against physical restraints
- Midazolam (Versed) 2.5 mg IV/IO OR
- Midazolam (Versed) 5 mg divided into 2.5mg each nare via MAD (mucosal atomizer device) or 5mg IM, if no IV access available
- chart vitals before and after administration when feasible
- OR
- Ketamine 1mg/kg IM (100mg max); or 0.5mg/kg IV (max 50mg)
- Chart vitals before and after administration when feasible
- If inadequate response or higher dose indicated Contact Medical Control
- Avoid if history of recent MAO inhibitor use (e.g. Phenelzine, Tranylcypromine)
- OR (when Ketamine is limited or unavailable)
- Droperidol 5mg IM or 2.5mg IV
- Chart vitals before and after administration when feasible
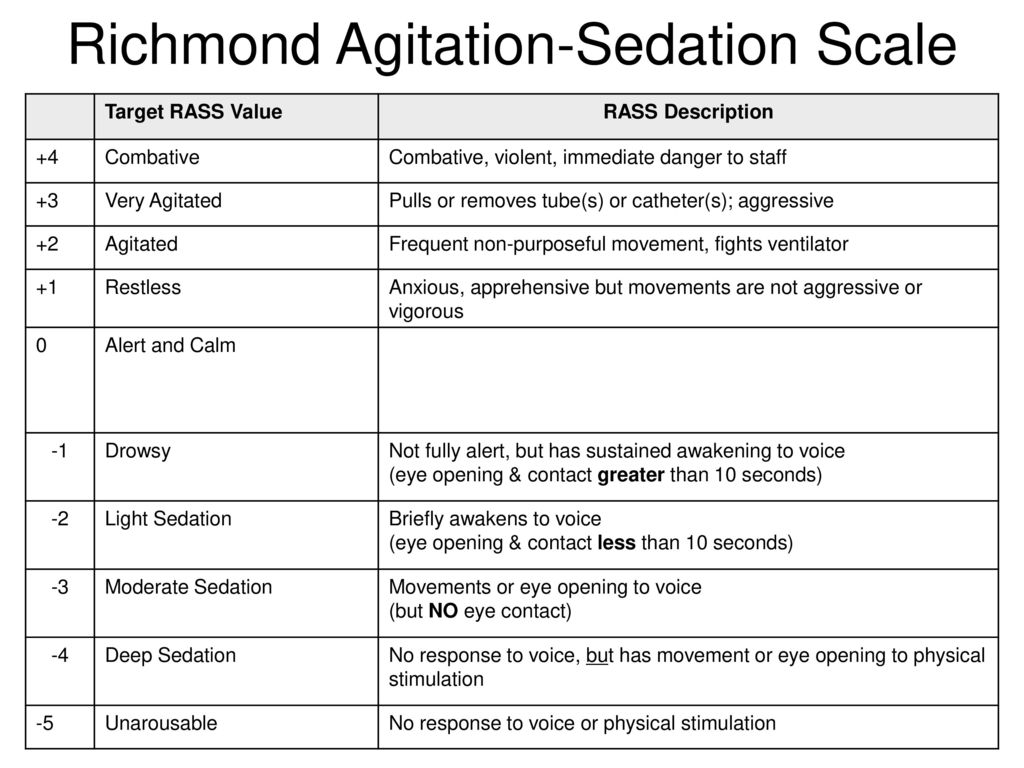
- If inadequate response (i.e. patient remains with a RASS of +3 or +4), an additional dose may be administered in 10 minutes.
- If cocaine/sympathomimetic toxicity strongly suspected:
- Midazolam (Versed) 2.5 mg IV/IO/IM or
- Midazolam (Versed) 5 mg divided into 2.5mg each nare via MAD (mucosal atomizer device) or 5mg IM if no IV access available
- Chart vitals before and after administration when feasible
- The following table is a reference for which you can consider utilizing to document level of sedation after medication administration.
Contact Medical Control for Additional Orders if Needed
Hypertensive Emergencies
A Hypertensive Emergency can be defined as systolic BP > 220 mm Hg and/or Diastolic BP >120 mm Hg, with evidence or symptoms of end organ damage. Prehospital treatment of isolated hypertension may result in critical reductions in target organ perfusion due to uncontrolled lowering of blood pressure. Focus on addressing the manifestations of hypertensive emergencies, such as chest pain or heart failure.
Basic Life Support
- Supplemental oxygen
- Including ETCO2 level (35-45 normal)
Advanced Life Support
- Full ALS Assessment and Treatment
- Provide supportive care
- For patients with chest pain, altered mental status, signs of stroke or pulmonary edema refer to the specific protocol
Contact Medical Control for Additional Orders if Needed
Hyperthermia
Basic Life Support
- Move patient to cooler environment
Heat Cramps
- Painful spasms of the extremities or abdominal muscles, normal mental status and vital signs
- Oral fluids as tolerated
- Sponge with cool water
Heat Exhaustion
- Dizziness, light-headedness, headache, irritability, normal or slightly decreased LOC, normal or decreased BP, tachycardia, normal or slightly elevated temperature
- Keep patient supine
- Supplemental 100% oxygen
- Including ETCO2 level (35-45 normal)
- Remove clothing
- Sponge with cool water and fan
Heat Stroke
- Marked alteration in LOC, extremely high temperature (often > 104), may be sweating but usually have red/hot/dry skin
- Position semi-reclining with head elevated 15-30°
- Supplemental 100% oxygen
- Including ETCO2 level (35-45 normal)
- Rapid cooling:
- Cold packs to axilla, groin and neck
- Sponge with cool water and fan
- If significant shivering occurs remove cold packs but continue fanning
Advanced Life Support
- If symptoms moderate to severe perform Full ALS Assessment and Treatment
- Hyperthermia may result from cocaine or other sympathomimetic toxicity:
- If cocaine/sympathomimetic toxicity strongly suspected see Cocaine and Sympathomimetic Overdose Protocol
- Emergency transport to nearest facility
Contact Medical Control for Additional Orders if Needed
Hypothermia
Basic Life Support
- Remove Wet Garments
- Protect against heat loss and wind chill
- Maintain horizontal position
- Avoid rough movement and excess activity
- Mild Hypothermia, >32° C (90° F)
- Passive re-warming
- Active external re-warming (heating blanket)
- Moderate 30-32° C (86° - 90° F) and severe ≤ 29° C (84° F)
- Avoid external re-warming
Advanced Life Support
- Full ALS Assessment and Treatment
- For patient in cardiac arrest
- If temperature ≤ 29° C (≤85° F)
- Continue CPR
- Withhold IV medication until temperature > 30° C (86° F)
- Limit shocks for VF/VT to a Max. of 3 until temperature > 30° C (86° F)
- If temperature ≥ 30° C (86° F)
- Continue CPR
- Give IV medication as indicated
- Repeat defibrillation for VF/VT as temperature rises
- If temperature ≤ 29° C (≤85° F)
Contact Medical Control for Additional Orders if Needed
Pain Management - Adult
Basic Life Support
- Assess baseline pain level (0-10 scale), (0 = No pain, 10 = Worst pain)
Advanced Life Support
Analgesic agents may be administered under standing orders for patients experiencing severe pain from any one of the following:
- Isolated extremity injury (examples below):
- Fractures/dislocations of the shoulder and upper extremity
- Fractures/dislocations of the hip and lower extremity
- Animal bites or envenomations to the extremities
- Tourniquet use
- Burn without airway, breathing, or circulatory compromise
- Sickle cell crisis with pain that is typical for that patient’s disease
- Severe back pain
- Acute chest pain, in accordance with Chest Pain protocol
- Kidney stone highly suspected, in accordance with Abdominal Pain protocol
Agent for Pain Control
- Fentanyl (Sublimaze) 1 mcg/kg (maximum 100 mcg) slow IV; repeat once after 5 minutes as needed (maximum 200 mcg total dose) OR 100 mcg intranasal via MAD (divide dose equally between each nare) Maximum cumulative dose is 200mcg
- Contraindicated if systolic blood pressure < 100 mmHg
- Preferentially use intranasal delivery via MAD for those where IV access may be difficult to obtain in a timely fashion (extremity burns/injuries) or not indicated for chief complaint.
- After each drug dosage administration:
- Reassess the patient’s pain
- Note adequacy of ventilation and perfusion
- Assess vital signs and mentation
- Actively monitor oxygen saturation & waveform ETC02
Contact Medical Control for Additional Orders if Needed
Sedation / Sedative Agent Use
It is not always possible to predict how patients will respond to receiving a sedative medication. This protocol is to be used in conjunction with any protocol that involves the use of medication which may result in sedation. Authorized medications that may result in sedation are Fentanyl, Midazolam, Ketamine, Etomidate, and Diphenhydramine.
Mild sedation
A drug induced state in which patients respond normally to verbal commands. Although cognitive function and coordination may be impaired, ventilatory and cardiovascular functions are unaffected.
Moderate sedation
A drug-induced depression of consciousness during which patients respond purposefully to verbal commands, either alone or accompanied by light tactile stimulation. Airway patency, spontaneous ventilations, gag reflex and cardiovascular function are maintained.
Deep Sedation
A drug induced depression of consciousness, during which patients cannot be easily aroused but respond purposefully after repeated or painful stimulation. The ability to independently maintain ventilatory function may be impaired. Patients may require assistance in maintaining a patent airway and spontaneous ventilations may be inadequate.
Sedative agent use should ideally result in minimal or moderate sedation only.
Advanced Life Support
- Continuously monitor the following:
- Patency of airway
- Vital signs
- Oxygen saturation and capnography
- Cardiac rhythm
- Level of consciousness and ability to follow commands
- Assure that appropriate equipment and personnel are immediately available for care and resuscitation if problems arise
- Document the indications for sedation
Contact Medical Control for Additional Orders if Needed
Seizure
Basic Life Support
- Supplemental 100% oxygen if active seizures
- Including ETCO2 level (35-45 normal)
- Nasal cannula is sufficient if no active seizures and no respiratory signs or symptoms
- Protect patient from injury
Advanced Life Support
- Full ALS Assessment and Treatment
- Blood glucose measurement
- If < 70 mg/dL, treat per Altered Mental Status/Hypoglycemia Protocol
- For active seizures do NOT delay treatment to obtain intravenous access, begin with IM dose unless IV is already established; consider IO/IN
- Administer Midazolam (Versed) 5 mg IM or intranasal via MAD OR 2.5 mg IV
- If seizures continue or re-occur repeat Midazolam (Versed) 5 mg IM or intranasal via MAD OR 2.5 mg IV; wait at least 5 minutes from initial dose
- If hypoxic seizures, drug induced seizures, seizures from head trauma, stroke or eclampsia are suspected, treat as above and refer to appropriate protocol for further care
- If patient becomes combative or agitated in the post-ictal state (after seizure resolution)
- Apply physical restraints as needed to ensure patient/crew safety (only as directed in Behavioral Emergencies protocol)
- If chemical restraints are required:
- Midazolam (Versed) 5 mg IM or intranasal via MAD OR 5 mg IV (total maximum dose including treatment for seizures is 10 mg IM/intranasal or 5 mg IV)
- Contact Medical Control for further orders
Diazepam rectal gel (Diastat®)
Some patients with a diagnosed seizure disorder will have their own Diazepam rectal gel (Diastat®) prescribed by their physician. When available, Diastat can be given if no IV is available. Use the patients prescribed dose or refer to the table below. If an IV is readily available, Midazolam is the preferred medication.
|
For patients > 12 years old (0.2mg/kg) |
||
|
Weight |
Dose |
|
|
(kg) |
(lbs) |
(mg) |
|
14-27 |
30-60 |
5 |
|
28-50 |
61-111 |
10 |
|
51-75 |
112-166 |
15 |
|
76-111 |
167-244 |
20 |
Contact Medical Control for Additional Orders if Needed
Sepsis
Sepsis is a rapidly progressing, life threatening condition due to systemic infection. Sepsis must be recognized early and treated aggressively to prevent progression to shock and death. Sepsis can be identified when the following markers of the Systemic Inflammatory Response Syndrome (SIRS) are present in a patient with suspected infection:
- Temperature > 38° C (100.4° F) OR < 36° C (96.8° F)
- Respiratory Rate > 20 breaths/min
- Heart Rate > 90 beats/min
- White blood cell count > 11 or < 4 (if available)
In addition to physiologic markers of SIRS, severe sepsis may cause hypoxia and inadequate organ perfusion, resulting in metabolic acidosis marked by decreased ETCO2 levels (measured by capnography)
Sepsis Alert
The purpose of a Sepsis Alert is to provide pre-arrival Emergency Department notification in order to facilitate rapid assessment and treatment of a suspected severe sepsis patient. A Sepsis Alert will be instituted for patients meeting 2 of the vital sign criteria below. Also, a sepsis alert should be initiated for patients with a suspected infection PLUS signs of end organ damage (altered mental status, respiratory distress, hypotension, decreased urination) even if vital sign criteria is not met.
- Two or more of the following:
- Temperature > 38° C (100.4° F) OR < 36° C (96.8° F)
- Respiratory Rate > 20 breaths/min
- Heart Rate > 90 beats/min
- ETCO2 ≤ 30 mmHg
- Signs of end organ damage (altered mental status, respiratory distress, hypotension, decreased urination) are criteria for severe sepsis therefore presence of these signs along with suspected infection should be sepsis alerted
Note: if patient does not meet criteria, consider alert based on paramedic discretion
Basic Life Support
- Supplemental 100% Oxygen
- Including ETCO2 level (35-45 normal)
Advanced Life Support
- Full ALS Assessment and Treatment
- Including ETCO2 level (35-45 normal)
- Notify hospital of incoming Sepsis Alert prior to arrival
- IV 0.9% NaCl- Administer if evidence of hypoperfusion (hypotension, altered mental status, delayed capillary refill, HR>110) and no signs of fluid overload
- Administer 500 ml boluses if HR>110, altered mental status, or delayed capillary refill
- Administer 500 ml boluses until systolic BP > 90 mmHg
- Total amount of IVF should not exceed 2000 ml
- Boluses may be given in rapid succession if systolic remains < 90 mmHg
- If systolic BP remains < 90 mmHg after 1000ml total fluid bolus
- Norepinephrine infusion at 0.5-16 mcg/minute IV/IO, titrated to maintain SBP > 90 mm Hg (see pg. 10-27 for infusion preparation chart) OR
- Push dose epinephrine: Remove 9ml (0.9mg) of 1:10,000 Epinephrine from the pre-filled syringe then draw 9ml of NS into the pre-filled syringe and mix solution. Concentration 10mcg/ml. IV push 1ml every minute to increase blood pressure to 90 mmHg; max 10ml (100mcg).
Contact Medical Control for Additional Orders if Needed
Shock
Shock is defined as a state of inadequate organ perfusion and tissue oxygenation. It is evidenced by the presence of any of the following signs and symptoms:
- Hypotension
- Narrow pulse pressure
- Tachypnea
- Tachycardia
- Delayed capillary refill
- Mottled skin appearance
- Diaphoresis
- Cool clammy skin
- Pallor
- Altered mental status
Signs and symptoms vary depending upon the stage of shock, which may be compensated (normal perfusion maintained) or decompensated (unable to maintain normal perfusion).
Categories of Shock
- Obstructive shock: Caused by an obstruction that interferes with return of blood to the heart. Examples include tension pneumothorax, cardiac tamponade, and massive pulmonary embolus.
- Hypovolemic shock: Caused by decreased blood or water volume. Hypovolemic shock may be hemorrhagic or non-hemorrhagic.
- Distributive shock: Caused by abnormal distribution of blood resulting from vasodilation, vasopermeability or both. Distributive shock may result from anaphylactic reactions (anaphylactic shock), sepsis (septic shock), or spinal cord injury (neurogenic shock).
- Cardiogenic shock: Cardiogenic shock is a result of cardiac pump failure, usually caused by severe Left Ventricular failure. May result due to massive MI.
Perform the following in conjunction with protocols that apply to the specific etiology of the shock state (e.g. trauma, allergic reaction, STEMI, sepsis, etc.):
Advanced Life Support
- Full ALS Assessment and Treatment
- Record & monitor continuous 02 saturation and microstream capnography
- Do not delay transport for IV insertion
- IV 0.9% NaCl en route
- Administer 500ml (250ml for cardiogenic shock) boluses until systolic BP > 90 mmHg
- Total amount of IVF should not exceed 2000 ml (1000 ml for chest trauma)
- Boluses may be given in rapid succession if systolic remains < 90 mmHg
- If systolic BP remains < 90 mmHg after 1000ml total fluid bolus
- Norepinephrine infusion at 0.5-16 mcg/minute IV/IO, titrated to maintain SBP > 90 mm Hg (see pg. 10-27 for infusion preparation chart) OR
- Push dose epinephrine: Remove 9ml (0.9mg) of 1:10,000 Epinephrine from the pre-filled syringe then draw 9ml of NS into the pre-filled syringe and mix solution. Concentration 10mcg/ml. IV push 1ml every minute to increase blood pressure to 90 mmHg; max 10ml (100mcg).
Contact Medical Control for Additional Orders if Needed
Stroke - Suspected
Central Florida Stroke Centers:
- Advent Health-Orlando (Comprehensive)
- Advent Health-Kissimmee (primary)
- Advent Health Hospital-Celebration (Comprehensive)
- Osceola Regional Medical Center (Comprehensive)
- Poinciana Medical Center (Primary)
- P. Phillips Hospital (Primary)
- Orlando Regional Medical Center (Comprehensive)
- Holmes Regional Medical Center (Primary)
- Lakeland Regional Medical Center (Primary)
- Heart of Florida Regional Medical Center (Primary)
- Tampa General Hospital (Comprehensive)
- Lake Wales Medical Center (Primary)
- Lawnwood Regional Medical Center (Primary)
- Indian River Medical Center (primary)
Basic Life Support
- Supplemental oxygen via nasal cannula only if O2 saturation ≤ 94%
- Maintain O2 sats above 94%
- Including ETCO2 level (35-45 normal)
- Obtain blood glucose level
- Keep head of stretcher at 30-45° elevation (unless spinal trauma suspected)
- If spinal immobilization is indicated, elevate head of backboard 15°-30° (reverse Trendelenburg)
- Give nothing by mouth
- Obtain family/caregiver contact information
- Document time last seen normal
Advanced Life Support
- Full ALS Assessment and Treatment
- Establish two large bore IV’s ( ≥ 18ga) in A/C region
- If unable to establish two, at a minimum at least one large bore IV (≥ 18ga) in the A/C region
- For hypotension (systolic BP < 90 mmHg) not improved by fluid boluses, or when fluid boluses are contraindicated
- Norepinephrine infusion at 0.5-16 mcg/minute IV/IO, titrated to maintain SBP > 90 mm Hg (see pg. 10-27 for infusion preparation chart) if available OR
- Push dose epinephrine: Remove 9ml (0.9mg) of 1:10,000 Epinephrine from the pre-filled syringe then draw 9ml of NS into the pre-filled syringe and mix solution. Concentration 10mcg/ml. IV push 1ml every minute to increase blood pressure to 90 mmHg; max 10ml (100mcg).
- If hypoglycemic (Blood glucose <70):
- Dextrose 10% 100ml IV/IO, (repeat in 10 minutes if BGL remains < 60 mg/dl) max of 250ml
- If no IV available:
- Glucose paste or other oral glucose containing agent (e.g. orange juice) if patient alert enough to self-administer oral agent
- If unable to take oral glucose administer Glucagon 1 mg IM/IN
- Complete Stroke Alert Screen:
- Stroke Alert Screen should also be performed on patients who complain of dizziness or unsteadiness
-
- If ALL of the following criteria are met initiate Stroke Alert:
- The patient has no evidence of trauma
- The stroke symptoms are new, and onset ≤ 24 hours or wake up stroke
- The initial blood glucose is ≥ 50
- The patient currently has an abnormal Stroke Examination
- If patient meets Stroke Alert criteria immediately notify the receiving Stroke Center
- Transport all Stroke Alert patients to the nearest Comprehensive Stroke Center.
- Consider air transportation if transport time will be > 20 minutes or paramedic discretion and also need for additional resources
- Account for traffic and time of day (applies to stroke, STEMI, and Trauma protocol)
- If patient does not meet Stroke Alert criteria, transport to closest appropriate facility
- If ALL of the following criteria are met initiate Stroke Alert:
- If seizures occur, refer to seizure protocol
|
Stroke Alert Screen (if all items “YES”, initiate Stroke Alert) |
||
|
Screening Item |
YES |
NO |
|
Absence of Trauma |
||
|
Stroke symptoms ≤ 24 hours or wake up stroke |
||
|
Initial Glucose ≥ 50 |
||
|
Abnormal Stroke Exam (Below) |
||
| If any screening item is “NO”, do not initiate Stroke Alert | ||
|
Stroke Examination |
|
|
Facial Asymmetry:
|
NORMAL (No facial droop) |
|
RIGHT WEAKNESS OR DROOP |
|
|
LEFT WEAKNESS OR DROOP |
|
|
Arm Drift:
|
NORMAL (Both arms held at same level) |
|
RIGHT ARM DRIFTS DOWN |
|
|
LEFT ARM DRIFTS DOWN |
|
|
Speech:
|
NORMAL (Clear and appropriate) |
|
SLURRED SPEECH |
|
|
INAPPROPRIATE WORDS |
|
|
UNABLE TO SPEAK |
|
| Do not initiate Stroke Alert if all Stroke Exam items are NORMAL | |
*In addition to the screening above, perform finger to nose testing of both hands. If unable to perform, initiate stroke alert.
Transport patient to a Comprehensive Stroke center if patient presents with sudden worst ever headache with sudden & unexplained decreased LOC, especially if associated with exertional activity, severe nausea/vomiting, neck discomfort with movement, GCS <15, or significantly elevated bp. These symptoms are concerning for severe ischemic or hemorrhagic stroke. Consider air transportation if transport time is anticipated to be > 20 minutes or paramedic discretion
*Account for traffic and time of day and also need for additional resources
Document the last time witnessed without deficit, as well as a name and telephone contact number for a relative/caregiver who can assist with medical decision making and additional history
Syncope
Basic Life Support
- Supplemental oxygen
- Including ETCO2 level (35-45 normal)
- Obtain blood glucose level
Advanced Life Support
- Full ALS Assessment and Treatment
- For hypotension (systolic BP < 90 mmHg) not improved by fluid boluses, or when fluid boluses are contraindicated
- Norepinephrine infusion at 0.5-16 mcg/minute IV/IO, titrated to maintain SBP > 90 mm Hg (see pg. 10-27 for infusion preparation chart) OR
- Push dose epinephrine: Remove 9ml (0.9mg) of 1:10,000 Epinephrine from the pre-filled syringe then draw 9ml of NS into the pre-filled syringe and mix solution. Concentration 10mcg/ml. IV push 1ml every minute to increase blood pressure to 90 mmHg; max 10ml (100mcg).
- Check blood glucose level
- If < 70 mg/dL, treat per Altered Mental Status/Hypoglycemia Protocol
- If ECG rhythm is bradycardia, heart block, or dysrhythmia, see specific protocol
- If Altered Mental Status persists, or if Acute Stroke suspected refer to appropriate protocol
Tracheostomy Complications
Basic Life Support
- Supplemental oxygen- can apply blow by O2 to tracheostomy
- Including ETCO2 level (35-45 normal)
- If ventilation inadequate (assessed by ETCO2, chest rise, & breath sounds), apply BVM to stoma or over nose and mouth while occluding the stoma (with a dressing)
Advanced Life Support
- If signs of obstruction, attempt to relieve by suctioning
- Always verify placement with ETCO2
- If patient is unable to be ventilated and the tracheostomy tube is dislodged, remove tube and replace (if stoma>6 weeks). If unable to replace or stoma < 6 weeks old, intubate orally and cover the stoma
- If unable to intubate, BVM over stoma or nose and mouth (occluding stoma)
- If there is significant bleeding, apply direct pressure. If bleeding continues, inflate the tracheostomy tube in an attempt to tamponade the bleeding (only cuffed tubes are able to be inflated).

