Pediatric Cardiac
Cardiac Arrest / Non-traumatic
Asystole and Pulseless Electrical Activity
Ventricular Fibrillation or Pulseless Ventricular Tachycardia
Bradycardia
Tachycardia
Sinus Tachycardia
SVT with severe cardiopulmonary compromise
Ventricular Tachycardia with a Pulse
Pediatric Cardiac Arrest General Approach
In the event a patient suffers cardiac arrest in the presence of EMS, the absolute highest priority is to apply the AED/Defibrillator and deliver a shock immediately if indicated. In the setting of cardiac arrest not witnessed by EMS, perform CPR immediately and continuously while setting up for rhythm analysis and delivery of shocks.
Airway management by BVM is sufficient in the pediatric arrest patient. A single attempt at intubation or laryngeal tube placement can be made if time allows, but should not interrupt chest compressions
Basic Life Support
- Check responsiveness
- Call “Patient Contact/Working code” time to dispatch
- Utilize pit crew approach
- Open airway, check breathing, and feel for pulse
- Assist ventilation with minimal interruptions in chest compressions
- 15:2 compression to ventilation ratio for BLS
- Apply AED and follow directions
- For children 8 years or younger use pediatric AED cables if available
- If shockable rhythm identified by AED:
- Administer shock and call “first shock” time to dispatch
- Resume CPR immediately after shock is delivered for 2 minutes
- Do not wait for pulse or rhythm check
- Re-analyze rhythm using AED and follow directions
- Continue assisted ventilation without chest compressions if pulse present
Advanced Life Support
- Advanced airway/ventilatory management
- Ventilation rate of 12-20 per minute (higher range for younger ages) with supraglottic or ETT, concurrent with compressions
- Follow algorithm for specific rhythm
- Establish peripheral IV or Intraosseous access
- All medications listed for IV use can be given IO
Cardiac Arrest / Non-traumatic - Pediatric
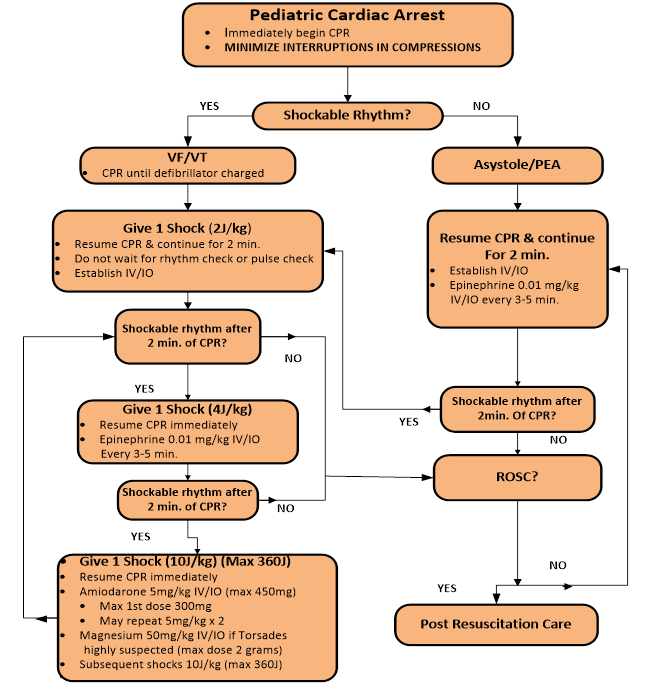
Cardiac Arrest - Asystole/Pulseless Electrical Activity
When asystole is seen on the cardiac monitor confirmation of the rhythm shall include a printed rhythm strip, as well as interpretation of the rhythm in more than one lead. Low amplitude V-Fib or PEA may be difficult to distinguish from asystole when using only the cardiac monitor display for interpretation.
Advanced Life Support
- Follow Cardiac Arrest-General Approach protocol
- Consider and treat possible causes
|
Potential Cause of Asystole |
Treatment |
|
Hypovolemia (most common cause) |
|
|
Hypoxia |
|
|
Hydrogen ion, acidosis (prolonged down time does not apply here) |
|
|
Hyperkalemia (end stage renal disease/dialysis) |
|
|
Hypothermia |
|
|
Toxins (drug overdose) |
|
|
Tamponade, cardiac |
|
|
Tension pneumothorax (all blunt trauma in cardiac arrest) |
|
|
Thrombosis, coronary |
|
|
Thrombosis, pulmonary |
|
- Epinephrine 1:10,000 0.01 mg/kg IV/IO every 3-5 min during arrest
- Drug overdoses (see specific drug OD/toxicology section)
Cardiac Arrest - Ventricular Fibrillation/Pulseless V-Tach
Advanced Life Support
- Follow Cardiac Arrest-General Approach protocol
- Defibrillate for persistent VF/VT:
- 2J/kg for initial biphasic shock (max 200 J)
- Continue CPR immediately after shock (do not stop to check pulse or rhythm)
- Call first defibrillation time to dispatch (if not done above)
- Analyze rhythm after 2 minutes of good CPR; If VF/VT persists:
- Defibrillate at 4J/kg (max 360 J)
- Continue CPR immediately after shock (do not stop to check pulse or rhythm)
- Epinephrine 1:10,000 0.01 mg IV/IO every 3-5 min during arrest
- Analyze rhythm after 2 minutes of good CPR; If VF/VT Persists:
- Defibrillate at 10J/kg (max 360 J); All subsequent shocks 10 J/kg
- Continue CPR immediately after shock (do not stop to check pulse or rhythm)
- Amiodarone 5mg/kg IV/IO bolus (max 300mg)
- For persistent VF/VT repeat Amiodarone 5mg/kg IV/IO bolus on second and third round (max total dose 15mg/kg)
- Or consider Lidocaine
- Lidocaine IV/IO initial dose: 1 mg/kg
- Follow with continuous IV infusion; may administer second bolus if delay between initial bolus and start of infusion is > 15-minutes.
- Continuous IV infusion: 20mcg/kg/minute. Per manufacturer, do not exceed 20 mcg/kg/minute in patients with shock, hepatic disease, cardiac arrest, or CHF
- Lidocaine IV/IO initial dose: 1 mg/kg
- Continue cycle of CPR & Drug --> Rhythm Check --> CPR --> Shock --> CPR and Drug --> Rhythm --> Check --> CPR --> Shock as needed
- Additional interventions to consider in special circumstances:
- Magnesium Sulfate 50mg/kg IV/IO if suspected Polymorphous VT (torsades de pointes) max of 2g
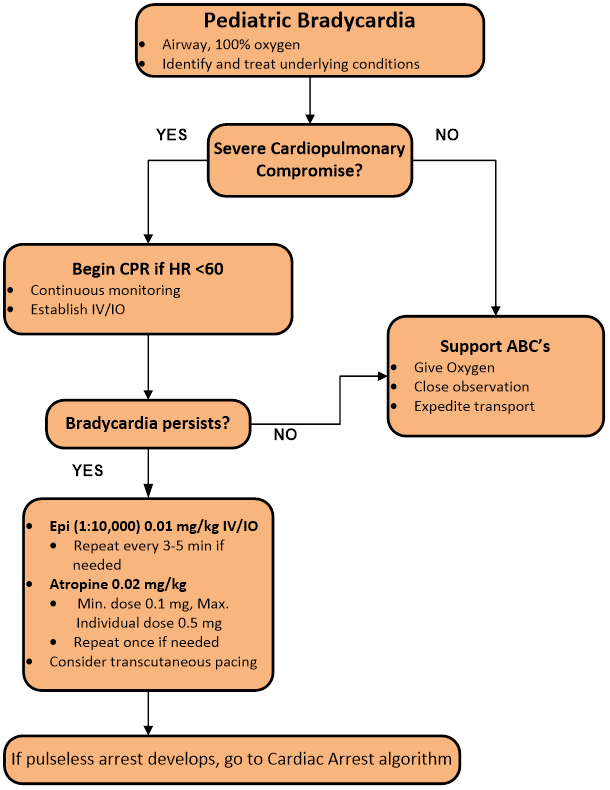
Cardiac Arrhythmias - Bradycardia
Basic Life Support
- Observe for signs of airway obstruction
- Bag valve mask with OPA/NPA ventilate; use only sufficient volume and force to just make chest rise visibly
- Ventilate at a rate of 12-20 breaths/minute, using the higher rate for younger ages
- Supplemental 100% oxygen
- Including ETCO2 level (35-45 normal)
Advanced Life Support
- Full Pediatric ALS Assessment and Treatment
- Identify and treat possible causes of bradycardia:
- If hypoxia open airway, assist breathing
- If hypothermic, re-warm
- If acutely deteriorating head injury, hyperventilate (goal ETCO2 of 30-35 mmHg)
- If heart block or post heart transplant, apply transcutaneous pacer
- If toxin ingestion, see specific toxin
- If hypoglycemic <70, administer Dextrose 10% 0.2gm/kg IV/IO (follow Hand Tevy guide)
- Obtain IV or IO access
- Do not delay treatment if patient is unstable by obtaining 12 lead ECG unless diagnosis is in question
- Stable Bradycardia: If HR<60 with adequate perfusion with no signs of shock, provide supportive care and expedite transport
- Unstable Bradycardia: If HR<60 with signs of poor perfusion (altered mental status, shock, or hypotension) despite supplemental O2 and ventilation:
- Perform CPR if less than 1 year of age
- Administer Epinephrine 0.01mg/kg 1:10,000 IV/IO; repeat q 3-5 minutes if no improvement
- Administer Atropine 0.02mg/kg IV/IO (single dose max 0.5mg, minimum dose 0.1mg), may repeat once
- Consider Transcutaneous Pacing if no improvement with above measures
- >15kg apply adult transcutaneous pacemaker
- <15kg use pediatric pads
- Use lowest energy setting that achieves ventricular capture
Cardiac Arrhythmia - Pediatric
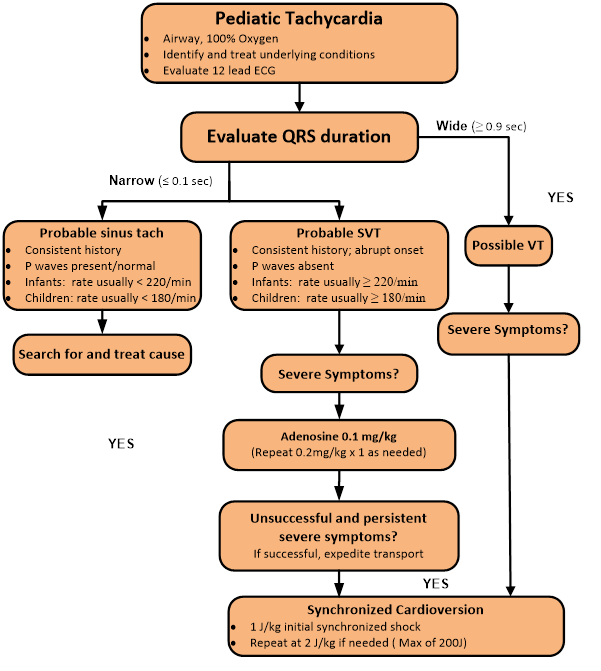
Cardiac Arrhythmias - Tachycardia
Basic Life Support
- Supplemental oxygen
- Including ETCO2 level (35-45 normal)
Advanced Life Support
- Full ALS Assessment and Treatment
- Obtain an EKG to distinguish between sinus tachycardia (p waves present), supraventricular tachycardia, and ventricular tachycardia (wide QRS)
Sinus Tachycardia
- Rate usually <220 for infants
- Rate usually <180 for children
- Identify and treat causes (hypovolemia, pain, fever, etc.)
Supraventricular Tachycardia (Symptomatic)
*Refer to HandTevy for up to date pediatric dosages
- Stable
- Vagal maneuvers
- Ice water, valsalva
- Adenosine Phosphate (Adenocard) 0.1mg/kg IV mg rapid over 1-3 seconds
- If no response in 2 minutes, 0.2mg/kg IV rapid IV over 1-3 seconds, twice as needed
- Unstable (hypotension, acutely altered mental status, or signs of shock)
- May give brief trial of Adenosine 0.1mg/kg rapid IV over 1-3 seconds if IV available
- Synchronized Cardioversion
- If no response 1J/kg
- If no response 2 J/kg (max individual dose 360J)
Ventricular Tachycardia with a Pulse
- Stable provide supportive care and expedite transport
- Unstable (hypotension, acutely altered mental status, or signs of shock):
- Synchronized Cardioversion
- If no response 1J/kg
- If no response 2J/kg (max individual dose 360J)
- Synchronized Cardioversion
- If Torsades de Pointes is suspected:
- Magnesium Sulfate 50 mg/kg IV over 10 minutes max of 2g